At 21 + 5 weeks’ gestation with a dichorionic diamniotic twin pregnancy, Shakina and Kevin presented at a community hospital with Shakina in threatened preterm labour. She was transferred to Mount Sinai Hospital, Toronto, for further evaluation and management of the pregnancy.
One hour after midnight, when Shakina reached 22 weeks’ gestation, she gave birth to Adiah, a girl, weighing 330 g. Her brother, Adrial, followed 23 minutes later, weighing 420 g. As Mount Sinai is one of a limited number of centres that provides resuscitation and active care at 22 week’s gestation, both infants received resuscitation support, which included mechanical ventilation.
After admission to the neonatal intensive care unit (NICU) at Mount Sinai Hospital, both twins had a complicated course, with challenges in their fluid management, skin management and ventilation, as well as complications of intraventricular hemorrhage and sepsis. Both twins had extremely thin, immature and transparent skin. Several neonatologists counselled Shakina and Kevin with regard to goals and direction of care, as prognosis at 22 weeks’ gestation is extremely guarded, especially for twins.
During the second week after birth, Adrial developed a spontaneous intestinal perforation, which prompted more discussions with parents regarding both short- and long-term prognosis. Adrial’s clinical instability prevented transfer to a surgical NICU, and his intestinal perforation was managed conservatively. He survived despite a serious systemic inflammatory process that followed the perforation and a blood stream infection. His skin was so immature and fragile that the percutaneous central venous catheter needed to be redressed every 12–24 hours, with extensive peeling of the skin with each redressing.
The parents stayed optimistic about their children. They clearly indicated that they wished for full active treatment and that they would accept any outcome. The NICU at Mount Sinai Hospital uses the Family Integrated Care Model, whereby parents are trained and integrated in the care provision for their preterm babies while the baby is in the NICU. Parents are involved in care provision as soon as feasible and for as long as possible, guided and supported by a multidisciplinary care team of nurses, physicians (consultants and trainees), nurse practitioners, respiratory therapists, social workers, pharmacists and dietitians.
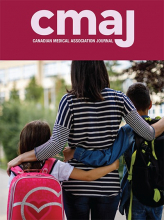
Both Adiah and Adrial survived and were discharged home after more than 160 days in the NICU. At the time of discharge, both were self-breathing on room air and were fully orally fed; neither infant required any technology support. They were assigned several follow-up visits with a pediatrician and at the developmental clinic, where they were seen by a developmental pediatrician, an occupational therapist, a physiotherapist and, based on need, a dietitian and a speech and language therapist. They were the youngest surviving twins by gestational age and birth weight ever treated at the Mount Sinai NICU; they are now 10 months old (or 6 months old, when corrected for prematurity) (Figure 1).
Babies Adiah and Adrial at 10 months old. Photograph by Shakina Rajendram and Kevin Nadarajah.
Image courtesy of Shakina Rajendram and Kevin Nadarajah
Parents’ perspectives
When I (Shakina) went into labour at 21 weeks’ and 5 days’ gestation, we were told that the pregnancy was a loss, and that nothing could be done to save the babies because they were “not viable.” All the hospital could offer was comfort care, which would involve placing the babies on us after they were born and waiting for them to die. There would be no other interventions to keep them alive. A nurse gave me a basin for the washroom to “catch” the babies if they “slipped out.” No words could capture the emotional, mental and physical trauma we experienced.
I (Kevin) recall being awake at 2:30 am, face streaming with tears, desperately asking God for a sign of hope. Shortly after, a close friend, Jennifer, sent me an Instagram account, TwentyTwo Matters, that advocates for 22-weekers and provides a list of hospitals that resuscitate them. Mount Sinai was on that list, and the next morning, our request for a transfer was accepted.
At Mount Sinai, we were informed that resuscitative efforts could not be pursued if the babies arrived before 22 weeks. We were warned that, even if the babies survived, they would have many disabilities affecting their quality of life. We acknowledged these risks and maintained our stance that the babies deserved a chance to live. Their quality of life would be determined not by the disabilities they might have, but by the love, nurture and support they received. Miraculously, the babies were born right after midnight, at 22 weeks’ and 0 days’ gestation, and were successfully resuscitated.
The first few weeks were the most heart-wrenching times of our lives. It was painful to watch Adiah and Adrial be subjected to numerous invasive procedures, pokes, tests and treatments. We watched both babies almost die in front of our eyes several times and were asked by doctors to consider when we would withdraw medical care for them. Although devastated, we reiterated that we would never stop fighting for our babies. Their lives were important and worth saving. While doctors were focusing on possible challenges, risks and outcomes in the future, we chose to focus on the progress the babies were making in the present, and to advocate for them every step of the way. It was always reassuring to speak to our nurses, social worker and other NICU parents who affirmed our decisions, and who helped us to stay positive and cling to hope in the darkest of days.
Even if there were limitations to the medical intervention the babies could receive, we believed other factors could substantially improve their outcomes. Our Christian faith is central to who we are, so we rallied friends and family from around the world to pray for our twins. We decided that, no matter how we felt, we would always smile, laugh, sing and celebrate every milestone with the babies. The Family Integrated Care Model allowed us to be fully involved in the babies’ care every day. They felt our presence and knew they were loved, which we believe made an important difference in their outcomes. The emotional, mental, financial, spiritual and physical supports we received from our friends, families and communities also made it possible for us to devote all our time and energy to our babies in the NICU for almost 6 months. Bringing our twins home was nothing short of a miracle. This journey has empowered us to advocate for the lives of other preterm infants like Adiah and Adrial, who would not be alive today if the boundaries of viability had not been challenged by their health care team. —Shakina Rajendram and Kevin Nadarajah
Primary nurse’s perspective
Health care providers who work in the NICU are often viewed by the public as miracle bearers, forerunners in medical advances, but little is publicized about their ethical dilemmas and personal struggles. For a period of my NICU nursing career, I struggled to determine whether I was a part of the solution or a part of the problem.
Medical advances have made it possible to redefine the age of viability. However, despite our greatest advances, NICU care carries its own challenges and risks. We may be able to sustain life, but we know that any complication may lead to permanent life-changing damages or even death. I often struggle not being able to know the negative consequences of our care with certainty, including not knowing if our life-sustaining care will delay the inevitable or result in survival with lifelong challenges. My struggle further intensifies when some parents lose interest in their own child’s care while also refusing withdrawal of care in the context of a grim prognosis, when it seems like our well-intended efforts lead to undesirable impacts to the family and perhaps even to society as a whole. Nature may be deterministic, but appropriate nurturing from everyone involved maximizes the preterm infant’s full potential. This was my perspective when Kevin and Shakina asked me to be one of their twins’ primary nurses.
My first encounter with the family was when the twins were in their first week of life. Kevin and Shakina showed no signs of withdrawal or sorrow, but rather a willingness to participate. Given the babies’ extremely small size and fragility, holding their babies as if they were full term was not possible yet. Instead, I encouraged them to wrap their hands around the baby inside the incubator as a means of hugging their baby and I captured their very first moment of bonding through photos and videos. When the twins were 4 weeks old, I noticed that the hand hugging picture was posted in front of the room. From that moment, I knew that these parents embraced every tiny moment of bonding with their children and I decided to be this family’s primary nurse, a role devised by our unit for neonates who are likely to stay in our unit for a long time. This meant that I would be assigned to take care of Adiah and Adrial on every shift that I worked until their discharge, to ensure a degree of consistency in care. I was informed of the many previous family meetings and of the parents’ determination to continue care. I was aware of the very intense care that had been provided, and that the future was unknown. I knew the road ahead would be treacherous for the family.
Both parents understood the situation well and were not in denial. Most families do not understand what at-home, 24-hour nursing care will entail for the child and the family. Most families dwell in the denial stage to cope with the devastating prognosis. Not every family can overcome the 5 stages of grief. This family reflected on the challenges ahead. They showed resilience and continued to be proactive, to learn and advocate for their children. It was Kevin and Shakina’s eagerness to overcome any challenges that inspired myself and the whole NICU team to let go of our personal struggles and dedicate our very best.
Throughout our 5-month nurse–family relationship, we engaged in some deep conversations. In one of these conversations, Shakina said, “We know that both Adiah and Adrial will go through their own developmental milestones at their different paces. We have agreed to teach our children to not celebrate their own milestones but to celebrate their sibling’s success. That way we can remind ourselves and our children not to compare themselves with one another but to be appreciative of every little or big achievement.”
In the NICU, we may not have all the answers, but I believe that we have made a positive impact in guiding these parents, off-loading some of their burdens and preparing them to address whatever challenges lie ahead. — Luzia Leong
Social worker’s perspective
Caring for twins born at 22 weeks’ gestation was a rocky unknown for our team. Meeting the parents for the first time, I wanted to focus on their experience. They shared what they were told with regard to resuscitation at this gestational age. Knowing how their children entered their lives at just the right time to be provided active care, by the difference of an hour, Shakina and Kevin chose to see this as the babies’ decision and wanted to help them fight for their lives. I talked about the usual aspects of Family Integrated Care that we practice, and I mentioned the importance of being present, talking to the babies, touching them and eventually participating in care, including skin-to-skin care. Kevin noted that I was the first person to talk about life and how they could be involved, rather than the likelihood of poor outcomes. This made me reflect on whether I was just following my routine introduction or whether I was being unrealistic. Should I have been more cautious? We reflected on this weeks later, and the parents shared that they were happy I did not stop myself, as our talk reaffirmed the hope they had in their babies’ survival.
Shakina and Kevin were present every day and participated in the babies’ care in all the ways possible. Yet, some team members worried the parents “weren’t getting it,” because they were so involved, instead of crying. This was frustrating as I saw the opposite, and advocated as such. I saw parents who were celebrating life, bringing positive energy, and staying grounded in the present, despite their distress with the situation. The parents told me they were not dreaming of the future, they were just trying to support their babies, and it was clear how much this task meant to them and how practical they were in their approach. Through team discussions during rounds, and with time, the team came to the same conclusion as me, which ultimately gave us a shared understanding of what the family was going through.
In the spirit of celebrating milestones, I brought the parents a “1 Week Old” milestone card after 7 days, which they loved. They shared how validating it was to have a team member celebrating the babies with them. Of course, there was doubt about the future, but they stayed present and celebrated whatever happened right in front of them, which I wanted to support. We had several family meetings about outcomes and whether to change the direction of care. They were steadfast in choosing full care and in optimizing the babies’ potential, and wondered how they could show their understanding without being mistaken for being idealistic. Having children born at such a young age is new terrain for any family. We talked about ways to communicate this collaboratively with the team; being able to do so gave them a new sense of empowerment about them. It was amazing to watch their confidence in care and advocacy grow as the babies grew. And just as they learned from us, we also learned a lesson in having a leap of faith and the impact of positive intention setting. — Sara Gambino
Neonatologist’s perspective
I received a call from a junior colleague regarding the resuscitation of twins at 21 weeks’ and 6 days’ gestation as Shakina was being transferred to us at Mount Sinai Hospital. My advice was to have a discussion with the parents to outline what it meant to have a baby born at this gestation — including short-and long-term outcomes — explain our technological capabilities, understand their expectations and make a mutually agreeable plan.
In Canada, most centres provide resuscitation and active intensive care only to neonates born at or after 23 weeks’ gestation, after consultation with the parents, because of the high rates of mortality and substantial neurosensory and developmental morbidity among survivors who receive this care before 23 weeks’ gestation. Debate regarding resuscitation at the age of viability is not new in neonatology, and the age of viability is constantly being challenged. The self-fulfilling prophecy of not providing active resuscitation and reporting no survival has generated challenging medical, ethical and moral discussions. Personal opinions, beliefs and the impetus to justify those opinions have made many health care providers portray a defensive or cautious outlook.
When I first met with Shakina and Kevin during the second week after Adiah and Adrial were born, I learned how concerned they were about the condition and progress of their children. In no uncertain terms, they indicated their unwillingness to withhold or withdraw life-sustaining care. However, their “hidden” concern was that they had been repeatedly questioned about their choice of pursuing full active care in the face of the most severe complications for their children. After this conversation, our care focus shifted to survival and the team understood the overall goals for this family. During that week, Adrial became severely ill with an intestinal perforation and an infection, and Adiah had substantial weight loss. These challenges could have resulted in death or survival with serious disabilities. However, both parents were hopeful and clutched to every single positive change in either of the twins and supported each other steadfastly.
My decision to be a neonatologist was primarily driven by the specialty’s capacity to constantly improve. None of us knew what the long-term consequences of the twins’ medical problems would be; however, one thing was certain — their parents would never give up hope. Many of my colleagues and team members kept asking, “Are we doing the right thing?”, “What are we trying to prove here?” and, most importantly, “Do the parents understand the challenges they’ll face in the future?” I wish I had those answers. I listened to the team’s concerns, and I tried to make everyone understand the parents’ perspectives during rounds. During my meeting with the parents, in the presence of their nurse and social worker, I fully supported their optimism while trying to make sure that I was not misleading them in any way.
One thing I knew without a doubt was that these parents were up to the task. I saw only unwavering hope, joy and pride in their eyes. The debate of resuscitation of periviable babies will continue; however, the lessons of humility that each family teaches me constantly remind me of the importance of integrating families in care, goal-setting and decision-making. I believe in guiding parents and families in this journey by trying to understand their beliefs, values and expectations. I support them as much as I can within the confines of what the team can actually offer their children at that time. — Prakesh S. Shah
360 Cases is a new type of Practice article that highlights the interpersonal and systemic aspects of health care that are seldom discussed in other Practice articles. Each comprises a brief case summary, followed by personal reflections from 2–4 people involved in the clinical encounter. One author must be a patient, family member or caregiver; the other authors may be anyone involved in the encounter (i.e., physicians, nurses, social workers, dietitians, etc.). For more information, see https://www.cmaj.ca/submission-guidelines or contact PatientEngagement{at}cmaj.ca.
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY-NC-ND 4.0) licence, which permits use, distribution and reproduction in any medium, provided that the original publication is properly cited, the use is noncommercial (i.e., research or educational use), and no modifications or adaptations are made. See: https://creativecommons.org/licenses/by-nc-nd/4.0/